Member Services Information
The ACME Health Benefits Plan is owned by its participants but is administered by Vault Administrative Services, powered by AMPS. Vault Admin Services ensures you receive fair pricing for your health services and prompt payment to your healthcare providers.

For Eligibility, ID Cards, Verification of Benefits, Medical Claims and Pre-Authorization:
Vault Admin Services / AMPS: 800-425-9374
Member Registration & Sign-in
Pharmacy Helpdesk:
877-403-4919
Questions regarding your pharmacy benefits?

Care Navigator:
800-425-9374
Find a providers in your local market, understand the claims process, learn what happens after the visit.

866-982-7988
edisonhealthcare.com
Looking to schedule a surgery or specialized medical treatment?
Member Resources: Frequently Asked Questions (FAQs)
Present your ACME Health Benefits card—just like any other health insurance plan you’ve used. You do not pay at the time of service.
Yes, of course! The best course of action is to call your provider to make the appointment, then call Vault Admin Services / AMPS to verify the benefits prior to the appointment, then be sure to take your card to your provider on your appointment day. And if you forget to call ahead of time to verify your benefits, that’s okay too.
Your healthcare provider should call 800-425-9374 (located on the back of your card) to validate and file using the information on the back of the card. A few weeks after your health service, you will receive an Explanation of Benefits (EOB) You are only responsible for the amount designated as ‘patient responsibility’ on the EOB.
If the provider bill states you owe more than the balance shown as ‘patient responsibility’ on the EOB, this is a ‘balance bill.’ Call AMPS immediately at 800-425-9374. A patient advocate will answer your questions and determine whether a dispute should be filed. Be sure to do this within 60 days of receiving the provider’s statement!
The AMPS Care Navigation team is there to help you find well-respected providers close to you to meet your needs. Mammograms, colonoscopies, MRIs, orthopedic procedures are all great examples of where Care Navigation can help you find the right provider. Call your Vault Admin Services / AMPS team at 800-425-9374.
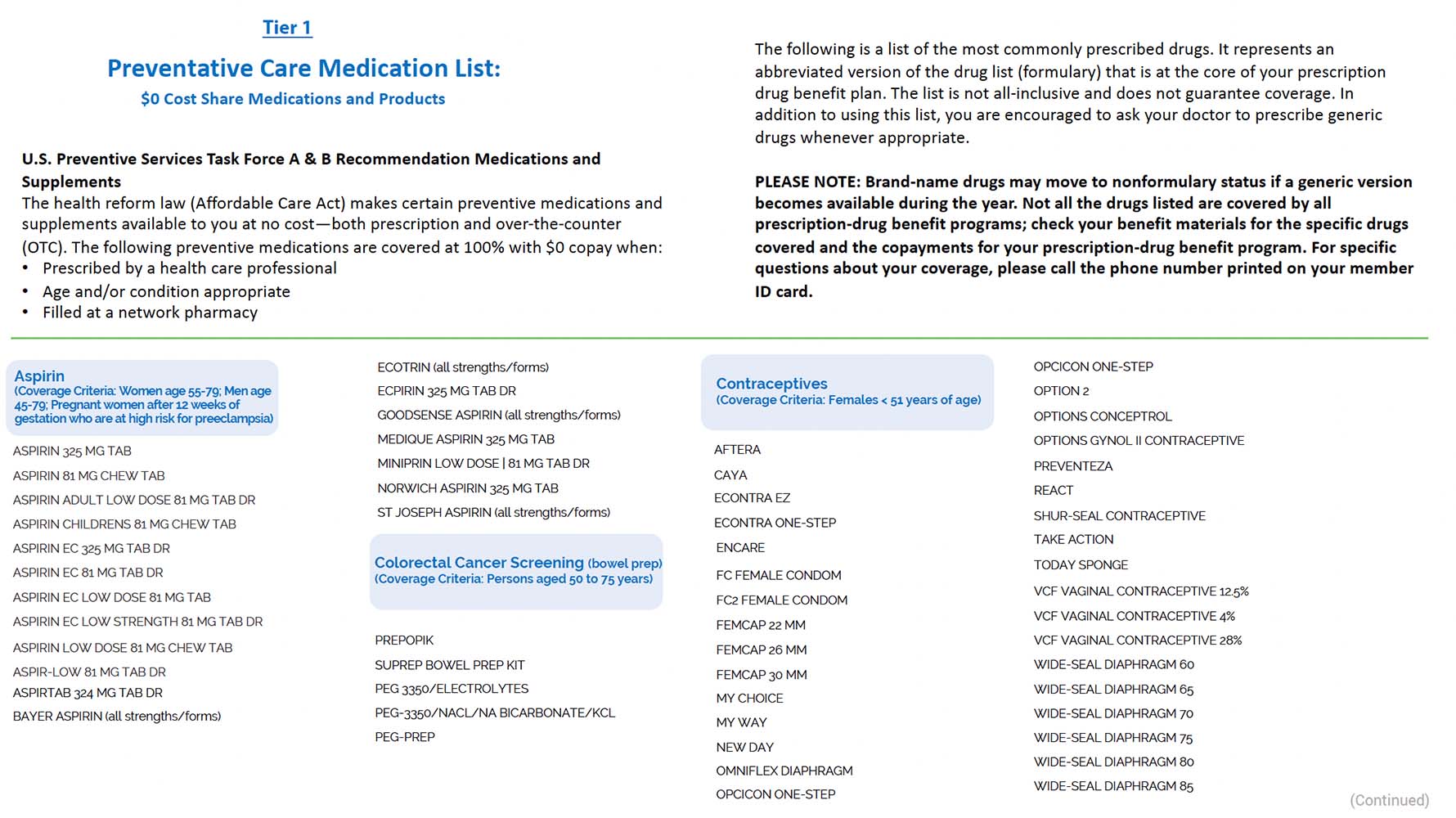
Your pharmacy benefits information will be on your benefits card. If you have specific questions about a particular prescription, call the pharma helpdesk at 877-403-4919. Have your card on-hand with your Bin and Group number.